Introduction
Acute abdominal pain is one of the most challenging urgent diagnostic pictures. Anamnesis, meticulous physical examination and basic complementary tests help in the diagnostic and therapeutic orientation of most processes. The greater use of abdominal computed tomography (CT) in this context has allowed the recognition of entities of rare appearance and conservative management such as epiploic appendagitis (EA).
Primary epiploic appendicitis or acute epiploic appendicitis is a benign inflammatory entity characterized by the presence of inflammation secondary to torsion or thrombosis of the venous drainage systems of the epiploic appendages, these structures are usually ocalized more commonly in areas adjacent to sigmoid colon.
EC is an uncommon cause of acute abdominal pain and its prevalence is unknown. It occurs most frequently between the fourth and fifth decade of life (70-85%), with a similar frequency between the sexes2. It constitutes between 2-8% of patients diagnosed with acute diverticulitis and 1% of patients with suspected acute appendicitis.
Medical history
A 66 year old female patient with a history of arterial hypertension, type 2 diabetes mellitus, hyperuricemia, migraine headache, cholecystectomy, had been studied two years before in the Surgery Service for recurrent abdominal pain in the left iliac fossa with a result of opaque enema within normality.
She went to the Emergency Department because for 20 hours she had presented localized abdominal pain in the left iliac fossa with irradiation to the epigastrium accompanied by abdominal distension, sudden onset, continuous, not related to ingestion or postural changes and without accompanying alterations of the intestinal habit (she referred to habitual constipation with occasional rectorrhagia in scarce quantity). There was no fever, nausea, vomiting or constitutional syndrome. No voiding syndrome.
Physical examination
The patient walks into the consultation, her vital signs in the triage consultation detect TA 122/78, heart rate 92 lpm, temperature 37.1ºC, presents good general condition, conscious, oriented, collaborative, good skin-mucosal coloration with good hydration. Eupneica. Cardiorespiratory auscultation does not show pathological findings. The abdomen is soft, depressible, painful in the left colic epigastrium-frame being the most painful palpation in the left iliac fossa, there was no abdominal defence, although there was a positive rebound sign in the painful point, the abdomen is somewhat distended, intestinal noises are diminished. Femoral pulses are present and symmetrical.
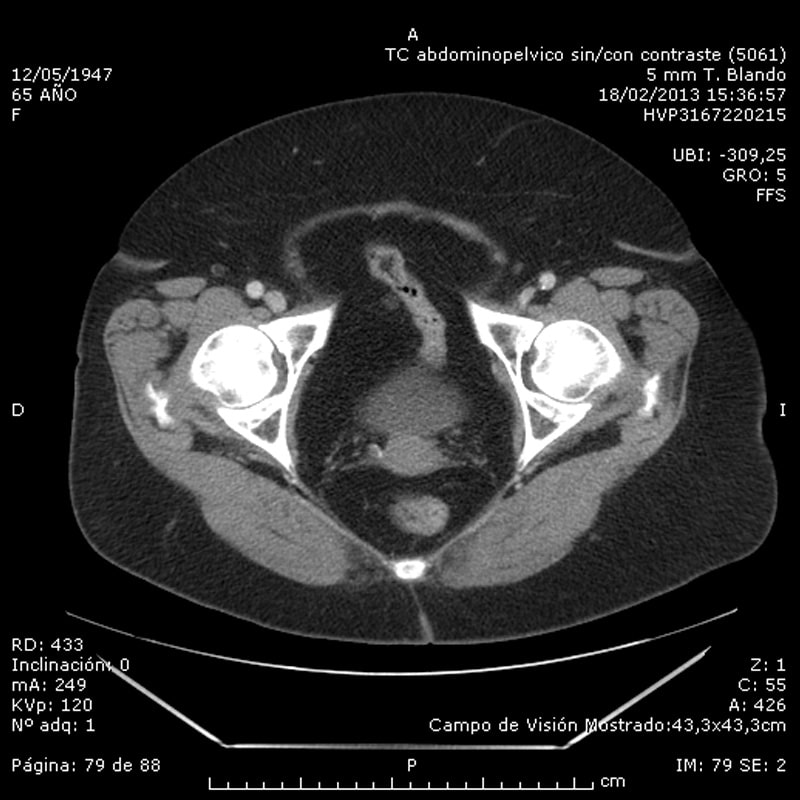
Computerized abdominal pelvic tomography
Complementary tests
Analytically, the blood count (leukocyte count and formula) and biochemistry (including bilirubinemia and amilasemia) remain normal. Surgical evaluation is requested for a CT scan of the abdomen showing torsion of a small epiploic appendix adjacent to the sigmoid colon. (fig. 1).
Differential diagnosis
Acute epiploic appendagitis, acute omental infarction, inflammatory processes (diverticulitis, appendicitis), sclerosing mesenteritis, primary or metastatic tumors involving mesocolon.
 Treatment and evolution
Treatment and evolution
Abdominopelvic computerized tomography Outpatient treatment is indicated with liquid diet, amoxicillin-clavulanic 500mg every 8h orally for 8 days and revision in external surgery consultation within 15 days.
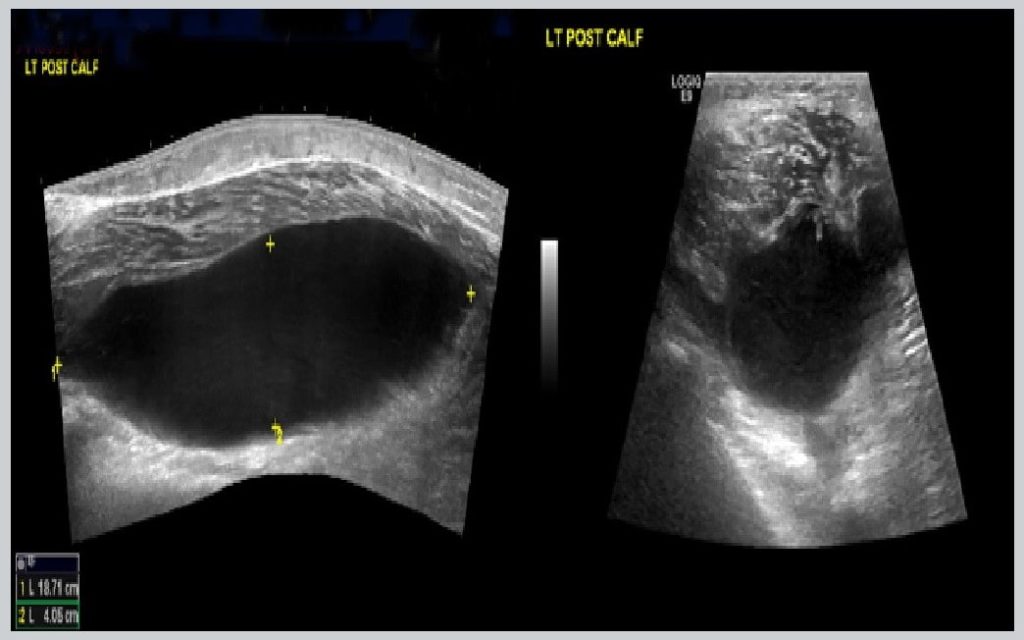
The patient goes to asymptomatic revision. The radiological control performed (abdominal CT contrast) was within normal range (fig. 2).
Discussion
Epiploic appendagitis (EA) is a benign entity debuting with a widely variable non-specific clinic. Analgesic treatment is usually of choice, with the need for surgical treatment being exceptional in these cases. The term epiploic appendicitis was introduced in 1956 by Lynn et al, and the characteristics of this process on CT were initially described in 1986 by Danielson et al. Until then the diagnosis was surgical1.
The most frequent location is in the sigma and descending colon followed by the ascending and transverse colon. It is not uncommon to detect it along the entire length of the colon, forcing differential diagnosis with multiple pathologies.
Sudden and intense pain in the lower left zone of the abdomen is usually the most common clinical manifestation, being able to simulate diverticulitis or appendicitis if it occurs on the right side. The presence of fever, nausea, vomiting or alterations of the intestinal habit is exceptional. The diagnosis is established with anamnesis, physical examination, analytical tests and basic radiology, ruling out other causes of acute abdomen. This leads to a broad differential diagnosis after them as omental infarction, mesenteric panniculitis, sclerosing mesenteritis or primary metastatic tumors of the mesocolon.
The diagnostic imaging technique is the abdominal CT very widespread and as a tool in the diagnosis of acute abdominal pain in the emergency is the most sensitive and specific test offering pathognomonic findings as in our case, the CT scan observed the epiploic appendix as a rounded image of fat density dependent on the serosa of the colon with circumferential protrusion of it and accompanied by thickening of the parietal peritoneum and / or wall of the colon. The treatment should be conservative by means of analgesics, oral anti-inflammatory and rest, with a tendency to the resolution of the picture not requiring surgical treatment or antibiotic guidelines. The prognosis of this entity is excellent, the clinical picture does not usually last more than two weeks although the radiological findings may persist from weeks to several months. Possible complications such as appendicular torsion, adherence to neighboring viscera, which may cause an abscess or intestinal obstruction, in which case surgical treatment must be performed, must be taken into account.
Conclusion
We must think of this rare entity when faced with a picture of abdominal pain fundamentally located in the flanks or iliac fossae. Epiploic appendagitis has characteristic ultrasound and CT findings which contribute to rapid diagnosis and therefore help with patient management. According to the findings, conservative behavior may be taken in patients with localized pain in one of the flanks without systemic symptoms or abnormal elevation of the white cell count.
Author: Joaquín Valle, MD
References
- Singh AK, Gervais DA, Hahn PF, Sagar PP, Mueller PR, Novelline RA. Acute epiploic appendagitis and its mimics. RadioGraphics 2005; 25: 1521-34.
- Legome EL, Belton AL, Murray RE, Rao PM, Novelline RA. Epiploic appendagitis: the emergency department presentation. J Emerg Med 2002; 22: 9.
- Sandrasegaran K, Maglinte DD, Rajesh A, Akisik FM. Primary epiploic appendagitis: CT diagnosis. Emerg Radiol 2004; 11: 9-14.
- A. González Vega, I. García Pérez, D. Álvarez Álvarez, A. Rizzo Ramos, J. L. García Muñiz, P. Pérez Ricarte. Epiploic appendagitis as aetiology of acute abdominal pain. Rev Esp Enferm Dig 2008; 100: 800-801.
- Singh AK, Gervais DA, Hahn PF, Sagar P, Mueller PR, Novelline RA. Acute epiploic appendagitis and its mimics. Radiographics 2005; 25: 1521-34.
- Horvath E, Majlis S, Sequel S, et al. Primary epiploic appendicitis: clinical and radiological diagnosis. Rev Med Chil 2000; 128: 601-7.