Abstract
Baker’s cyst is a closed collection of fluid that forms in the posterior aspect of the knee. Usually, it appears as a non -painful inflammation in the popliteal fossa. In adults, its aetiology is secondary to problems that cause distension of the knee joint; It is often associated with rheumatoid arthritis and osteoarthritis. Occasionally, the cyst may become oversized and rupture with the consequent leakage of synovial fluid into adjacent tissues, presenting a clinical course similar to acute thrombophlebitis. Infection of a popliteal cyst is an uncommon complication and is associated with septic arthritis. In this paper, we present the case of a patient, an intravenous drug user (IVDU), who developed a spontaneous infection of a Baker’s cyst secondary to Staphylococcus aureus, which was diagnosed in the emergency department (ED) using point–of–care–ultrasound (POCUS).
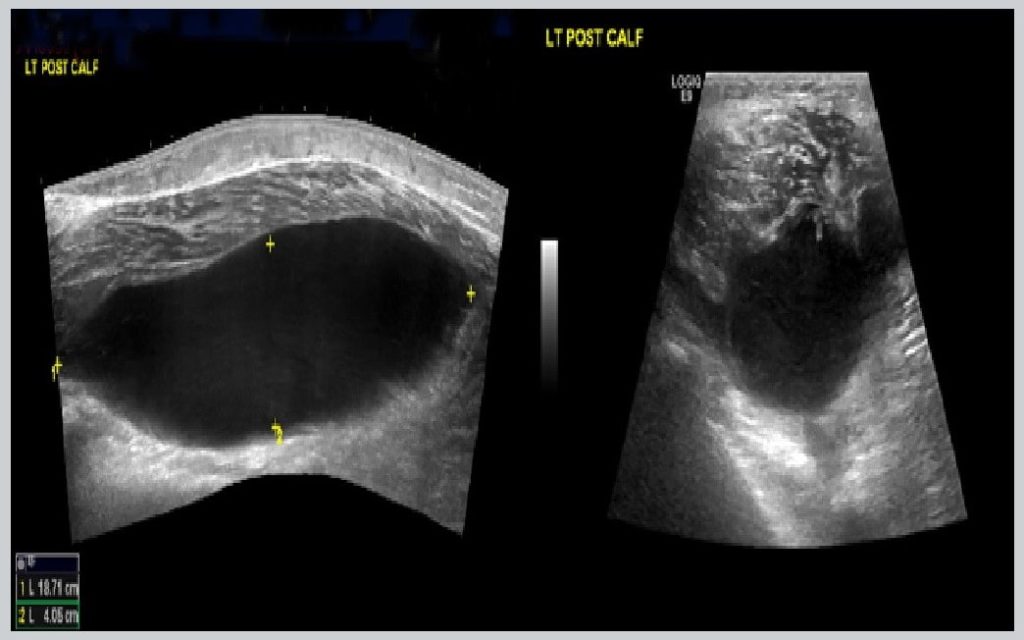
Figure 1. Within the posterior aspect of the left calf on the medial aspect there is an extremely large cystic lesion measuring 18.7 cm in length and 4 cm in width with no adverse features. The cystic lesion is communicating with the semimembranosus/medial head gastrocnemius bursa more proximally in the knee where it demonstrates internal echoes and synovial thickening and a single septation.
Introduction
A Baker’s cyst (also known as a popliteal cyst) is not a true cyst but a distension of the gastrocnemius semimembranosus bursa behind the knee [1]. In most cases, they appear between the tendons of the gastrocnemius and semimembranosus muscles on the medial side of the popliteal fossa, slightly distal to the centre crease of the knee [2]. Most Baker’s cysts are not associated with complications; however, the most common complication is rupture. This may be asymptomatic in up to 80% of people [3]. One uncommon complication is an infected popliteal cyst. [4].
Case report
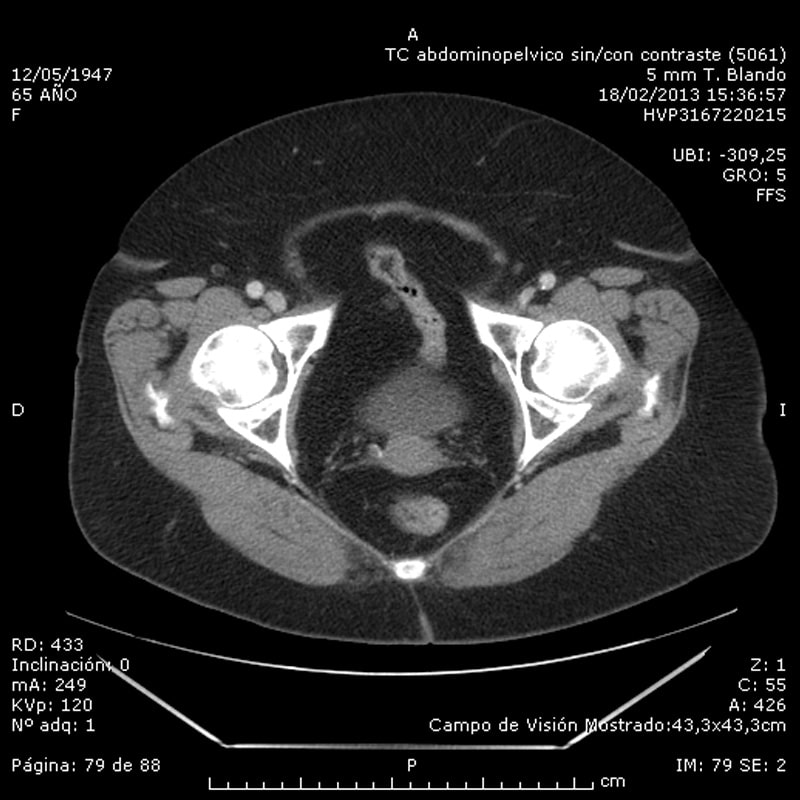
A 32-year-old man presented to the emergency department with a two-day history of acute onset of swelling and pain in the left calf. The patient had a history of hepatitis C, intravenous drug use with past admissions due to repeated soft–tissue abscesses at drug injection sites. The patient denied any trauma to the leg, and was not on any regular medication. On examination, there was marked swelling and tenderness in the left calf. He had a temperature of 37.7°C, a heart rate of 110 beats/min, a blood pressure of 110/707 mm Hg, and a respiratory rate of 18 breaths/min. A three-point compression point-of-care-ultrasound (POCUS) of the leg was performed which did not show any evidence of a DVT; however, a large cystic structure in the posterior aspect of the calf was identified (Figure 1). A knee ultrasound also demonstrated a fluidfilled area suggesting an associated knee effusion. A knee aspiration revealed a WBC count of 135 000 cells/µL, with 95% neutrophils (Figure 2). The patient was admitted under Orthopaedics with a suspected diagnosis of a septic knee and a ruptured infected Baker’s cyst. Blood test results at admission are shown in supplementary material (online Table S1). An inpatient Doppler ultrasound of the leg excluded DVT. A musculoskeletal ultrasound of the left leg confirmed the findings of an extremely large complex haemorrhagic or infected Baker’s cyst. The patient was initially treated with intravenous flucloxacillin. A knee aspiration culture revealed staphylococcus aureus. The patient was planned for surgical treatment however he self-discharged from hospital. The patient returned to Hospital 1 month later feeling unwell, pyrexial and complaining of pain in the right sternoclavicular area. Computerized tomography (CT) of the chest demonstrated acute septic arthritis of the right sternoclavicular joint with superficial phlegmon and small superficial ring enhancing collection anterior to the medial right clavicle and superiorly, appearances most likely secondary to Staphy-lococcus aureus. The knee swelling had improved, but symptoms were still persistent, however the patient refused any invasive treatment and accepted an intravenous course of Vancomycin.
Discussion
Infection of a Baker’s cyst is a very uncommon. The initial clinical suspicion of deep vein thrombosis or cellulitis is the most frequent clinical presentation [5]. The clinical signs suggestive of this infection are defined by a soft cyst, with a well–defined contour, located in the popliteal fossa and in the case of rupture, will lead to the appearance of a growing hematoma or anterior or distal ecchymosis of the lateral malleolus. Regarding diagnostic techniques, CT and magnetic resonance imaging (MRI) allow the cyst to be clearly defined, as well as to confirm rupture of the cyst along with any haemorrhagic complications, and whether it is accompanied by polymyositis or osteomyelitis. However, ultrasound can also easily detect a cystic structure in the popliteal fossa. Classically it can be identified as a well–defined cyst with a ‘neck’ at its deepest extent, extending into the joint space between the semimembranosus tendon and the medial head of the gastrocnemius. Identification of a fluid–filled structure at the posteromedial knee is suggestive of a popliteal cyst, but identification of the ‘neck’ between the tendons is necessary for a definitive diagnosis, the ‘neck’ has been described as being shaped like a “speech bubble” or “talk bubble” [6].
In cases of bacterial infection, the drainage of the capsule or cyst fluid usually shows the presence of purulent fluid. When Gram staining or bacterial culture of the aspirate is negative, investigation of a fungal or mycobacterial aetiology should be ruled out. Overall, the most frequently isolated infectious etiologic agent is Staphylococcus aureus, although it can be easily infected by other systemic infectious agents. Other detected organisms include; mycobacterium tuberculosis, candida albicans and streptococcus pneumoniae [7].
This case reflects the utility of POCUS in ED to evaluate patients with musculoskeletal complaints, in this case acute calf pain and swelling which is a common presentation in the ED. On initial presentation, a DVT was suspected. A three-point ultrasound demonstrated compressible femoral and popliteal veins with no obvious evidence of DVT, however a non–vascular image in the popliteal fossa was visualized measuring 24 cm, the cyst was communicating with the semimembranous and medial head gastrocnemius bursa, a knee effusion was also demonstrated. The case was discussed with the Orthopaedics team and a formal ultrasound was requested that confirmed the findings and suspected a ruptured infected Baker’s cyst which was supported by raised inflammatory markers and IV antibiotics were immediately started. In the past 10 years’ emergency physicians have improved the ability of musculoskeletal (MSK) ultrasound. POCUS can identify inflamed or fluid structures. POCUS has changed the management in 65% of patients with joint pain, erythema, and swelling and reduced planned joint aspiration from 72.2 to 37 % [8]. The skin, soft tissue, and most parts of the MSK system are relatively superficial anatomical structures and ideal targets for ultrasound examination. Using MSK POCUS, emergency physicians can provide better care to patients presenting with MSK complaints in the ED.
Conclusions
Using POCUS in ED, most of the differential diagnoses for acute calf pain and swelling can be identified with confidence.